Written by Laura Disenhaus, PT, DOMP, DScO
What is Pudendal Neuralgia?
Pudendal neuralgia is debilitating chronic nerve-related pelvic pain condition. Symptoms are characterized by pelvic pain, usually in the genitals or ano-rectal area that are typically made worse by sitting, and can occur on one or both sides. Pudendal neuralgia pain often feels like a stabbing, aching, burning, pinching, numbing, or bruised feeling in the genitals and anus.
Other symptoms include:
Pain during sex, having to pee more often, pain with peeing or with bowel movements, labial/vaginal pain, penis pain, difficulty reaching orgasm, and erectile problems/dysfunction. The pain can also spread into the thighs and back.
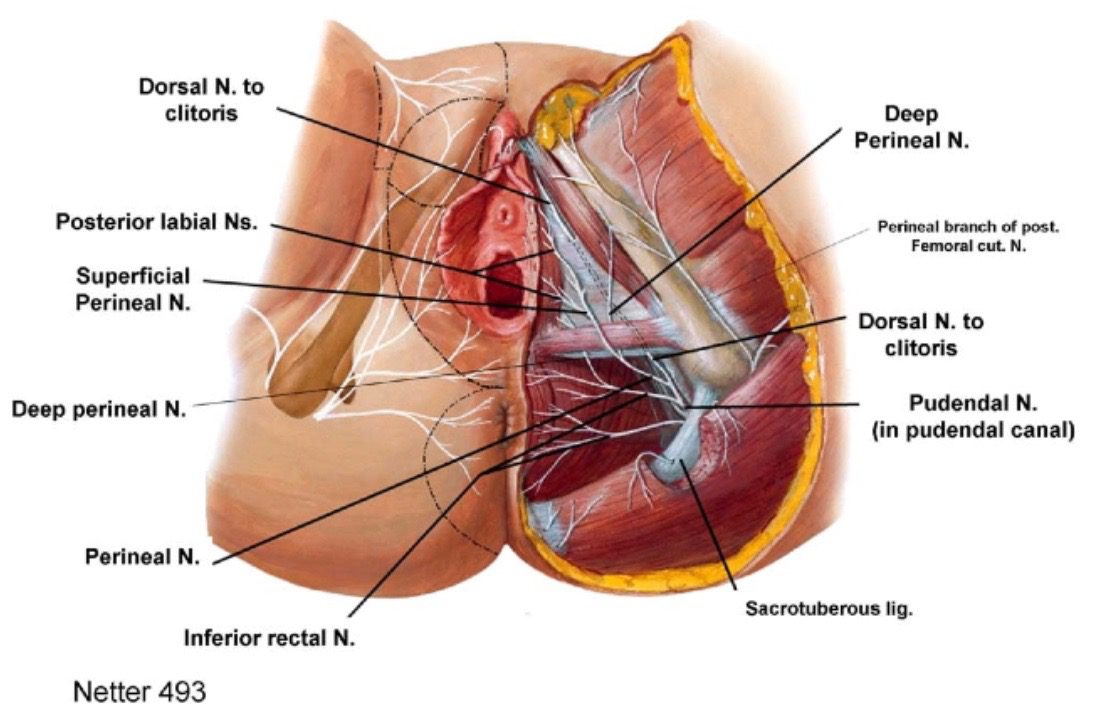
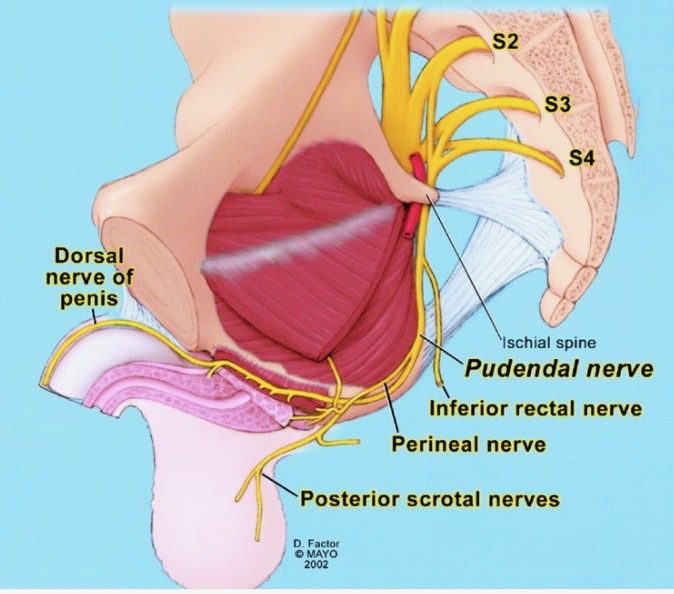
The images below show the pudendal nerve branches at the pelvic floor and the nerve as it is formed inside the pelvis.
What causes Pudendal Neuralgia?
The kinds of things that cause pudendal pelvic pain / pudendal neuralgia are usually the following:
– Regular prolonged sitting
– Activities that put chronic pressure on the sitting bones and tailbone areas such as long-distance cycling, and rowing,
– Tension or compression of the nerve from straining with constipation and prolonged or traumatic childbirth (eg. forceps, suction), and from other forms of exercise such as squats and weight-lifting
– Pelvic surgery due to stretching or compression of the nerve because of the surgery itself or from positioning for it.
There are four places where the pudendal nerve can be compressed or irritated:
- As it leaves the pelvis right beside the tailbone and passes by the piriformis muscle,
- As it passes the coccyx and is pressed between the sacrospinous and sacrotuberous ligaments,
- As it passes through the pudendal (Alcock’s) canal, a fascial tunnel formed by the obturatus internus fascia,
- At or after the nerve splits into its terminal branches to the genitals (perineal nerve, inferior rectal nerve, dorsal nerve of the clitoris or penis).
Getting diagnosed is key, so be sure to talk to your doctor to get properly diagnosed. There are effective treatments available including pelvic health physiotherapy.
How can Pelvic Floor Physiotherapy help me?
Pudendal nerve blocks, and surgical interventions are often prescribed for pudendal neuralgia.
But emerging research shows that pelvic health physiotherapy, with a focus on pelvic floor relaxation, is an effective, non-invasive approach to treating the condition.
Internal myofascial releases, relaxation and breath training, and specific exercises and to get the nerve gliding with movement are key to pelvic physiotherapy treatment.
How can Osteopathy help me?
Osteopathy is key for addressing the spinal and pelvic joints that are in relation to the pudendal nerve and need mobilizing. Visceral manipulation of the fascias around the pelvic organs can be very helpful in releasing tension along the nerve pathway. But osteopathy does not just assess and treat locally. There is a deep understanding of the fascial, circulatory, neural and functional relationships between the pelvis and the rest of the body. So areas that seem far away from the pelvis and the pudendal nerve may be affecting it. Osteopathy assesses the whole body, and then addresses those areas also.
I